As part of its June 15th report to the Congress, MedPAC included a chapter assessing the effects of the Hospital Readmissions Reduction Program (HRRP). The chapter responds to a mandate from the Congress (included in the 21st Century Cures Act) to study whether reductions in readmission rates under the HRRP caused increased utilization of outpatient and emergency services. Created by the Congress in 2010, the HRRP penalizes hospitals with high rates of readmission. After the implementation of the HRRP, readmission rates declined. However, some observers voiced concern that lower readmission rates led to offsetting growth in emergency department visits and outpatient observation stays. The Commission found that the HRRP contributed to declines in readmissions but has not caused material increases in outpatient observation stays or emergency department visits, nor has the HRRP had a net adverse effect on mortality.
Improving care transitions: The Hospital Readmissions Reduction Program (HRRP)
In 2008, MedPAC concluded that hospitals, physicians, and post-acute care providers needed to improve care transitions to reduce hospital readmissions and their associated harms (MedPAC 2008). Hospital readmissions pose significant risks for beneficiaries, including infection and medication error, and put beneficiaries through considerable physical and psychological stress (Rockwood 2012, Wilson et al. 2012, Klevens et al. 2007). In addition, readmissions increase Medicare spending, further straining the program’s finances (MedPAC 2013).
To create an incentive for hospitals to improve care transitions, the Commission’s June 2008 Report to the Congress recommended publicly reporting readmission rates and reducing payments to hospitals with rates that are relatively high (MedPAC 2008). In 2009, CMS began publicly reporting hospital-level readmission rates for acute myocardial infarction (AMI), heart failure (HF), and pneumonia. The following year, the Congress created the Hospital Readmissions Reduction Program (HRRP), which penalizes hospitals with higher-than-average readmission rates. The goals of the HRRP are to improve care transitions, relieve Medicare beneficiaries of the burden of returning to the hospital, and relieve taxpayers of the cost of readmissions.
The HRRP has been successful in preventing beneficiary harm and relieving taxpayer burden
Following the enactment of the HRRP, readmission rates declined, with conditions covered by the policy (AMI, HF, and pneumonia) experiencing the greatest declines. The Commission’s analysis found that between 2010 and 2016, readmission rates fell by 3.6 percentage points for AMI, 3.0 percentage points for HF, and 2.3 percentage points for pneumonia, compared with an average decline of 1.7 percentage points across all other conditions not covered by the policy. The Commission’s findings are consistent with an extensive literature showing declines in hospital readmission rates following the enactment of the HRRP (Birmingham 2018, Ibrahim et al. 2017, Cary et al. 2017, Zuckerman et al. 2016, MedPAC 2016).
Declining readmissions reflect real improvements in care
While there is broad consensus that readmission rates have declined, some have questioned whether the implementation of the policy has led to increases in substitute models of care, including outpatient observation stays and emergency department visits (Himmelstein and Woolhandler 2015).
The Commission found that observation stays did increase following the introduction of the program, but the increase was slight and offset only a small share of the reduction in readmissions. Therefore, the observed reduction in readmission rates likely reflects real change in practice patterns and not a shift of short-stay admissions to observation stays. The Commission also found that observation stays among patients without an initial hospital admission increased at a rate similar to that for patients with an initial hospital admission, suggesting that other policies enacted at the same time as the HRRP may have played a role in the slight overall increase in observation stays.
Emergency department visits also increased following the introduction of the HRRP. However, the Commission found that ED use increased during the 30 days following a hospital discharge both for conditions covered by the HRRP and for all other conditions. We also found that the use of ED services increased by a similar amount for beneficiaries who had not recently had a hospital stay. Indeed, the share of all ED visits that were post-hospital discharge visits was the same (4.8 percent) before and after the introduction of the HRRP. Thus, it appears that the growth in emergency room visits is a phenomenon largely unrelated to the HRRP.
The HRRP has not negatively affected mortality
Some researchers have raised the question of whether efforts to reduce avoidable readmissions have reduced necessary readmissions as well, resulting in higher mortality for heart failure (HF) patients. The literature is mixed on this question (Gupta et al. 2017, Dharmarajan et al. 2017). Above and beyond our mandate, to evaluate these claims, we examined HF mortality rates during the hospital stay and 30-days post-discharge from 2010 and 2016 (before and after the implementation of the HRRP). The results of three different analyses led the Commission to conclude that the HRRP has not increased mortality:
- On average, mortality after discharge from the hospital declined across all-HRRP covered conditions. Unadjusted pneumonia and AMI mortality decreased rapidly following the implementation of the program.
- Unadjusted HF mortality during the hospital stay and 30 days post-discharge increased between 2010 and 2016. However, these results can be misleading because they do not account for changes in the health status of beneficiaries. After adjusting for changes in health status, we found that mortality declined for all three conditions, including HF. Our analysis suggests that during this period there was a real increase in severity of illness among HF patients admitted to the hospital. From 2010 to 2016, there was a dramatic reduction in initial admissions to the hospital: HF admission rates per capita fell 14 percent, suggesting a change in practice patterns, with less severely ill patients treated on an outpatient basis, and more severely ill patients treated in the hospital. These more severely ill patients had higher risk of death. Thus, unadjusted mortality for HF patients who had a hospital stay was higher in 2016 than in 2010. But, after accounting for the sicker patient population, the Commission found that HF mortality rates actually declined over the period.
We also found that hospitals experiencing a decline in their readmission rates over the period also saw reduced mortality across all three conditions covered under the HRRP. On average, hospitals that achieved greater-than-average reductions in readmission rates also achieved slightly greater-than-average reductions in their mortality rates.
Figure 1: Risk-adjusted changes in unplanned readmission rates by condition
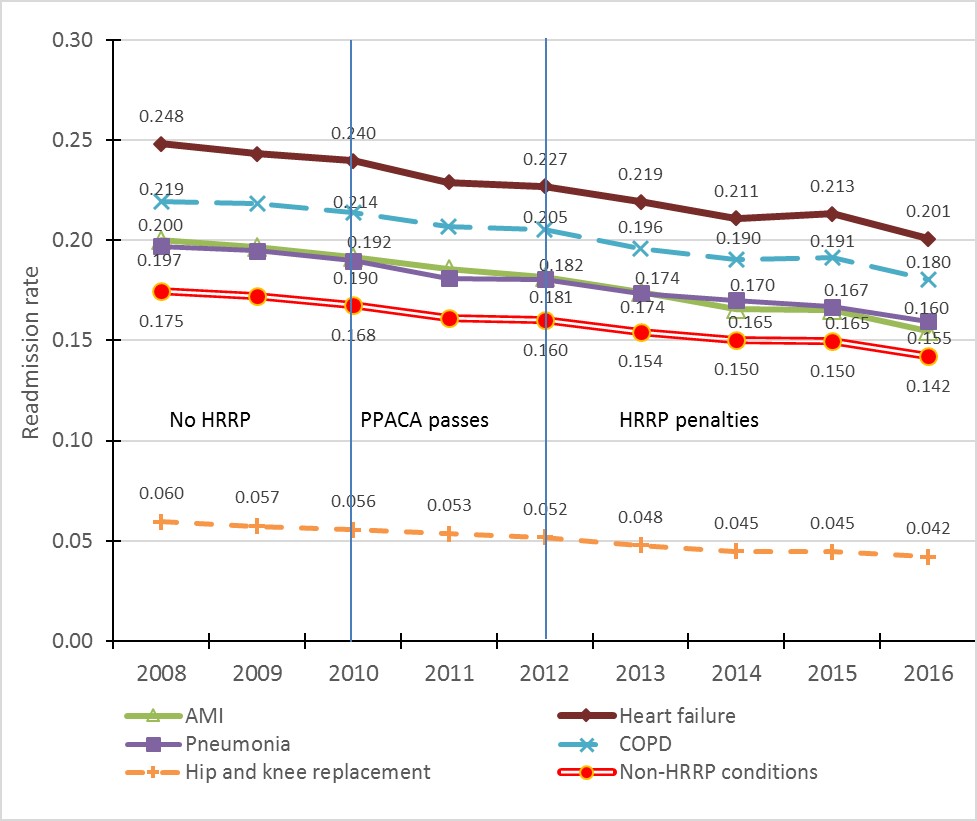
Note: HRRP (Hospital Readmission Reduction Program), PPACA (Patient Protection and Affordable Care Act of 2010), AMI (acute myocardial infarction), COPD (chronic obstructive pulmonary disease), Pneumonia measure reflects the expanded definition used starting in fiscal year 2016, which includes simple pneumonia, aspiration pneumonia, and sepsis with pneumonia as a secondary diagnosis.
Source: MedPAC analysis of 2008 through 2016 Medicare claims files for Medicare FFS beneficiaries age 65 or older.
The Commission found no evidence to suggest that the readmission policy has increased mortality. To the extent that there is any effect, our analysis suggests that the HRRP may have slightly helped to reduce mortality rates.
The HRRP has succeeded
In summary, the Commission’s findings suggest that the HRRP encouraged hospitals to place greater emphasis on reducing readmissions, and readmission rates declined as a result. The decline in readmissions across all conditions resulted in net savings to the Medicare program on the order of $2 billion per year. Importantly, beneficiaries had to endure fewer readmissions to the hospital. While the HRRP may have contributed slightly to a secular trend of increasing use of outpatient observation stays and emergency department services, the resulting small increases in costs for these services were far outweighed by the savings from reduced readmissions.
The HRRP has been a success thus far. However, improvements could be made to further refine and strengthen the program. In June 2013 MedPAC outlined budget-neutral policy options for how the HRRP could continue to be refined, including using fixed (rather than relative) performance targets, reducing penalties per excess readmission and expanding the HRRP to cover all conditions (rather than selected conditions), and improving how the program adjusts for socioeconomic status by evaluating performance using peer groups (MedPAC 2013, MedPAC 2018).
References
Birmingham, L.E., and W.H. Oglesby. 2018. Readmission rates in not-for-profit vs. proprietary hospitals before and after the Hospital Readmission Reduction Program implementation. BMC Health Services Research 18, no. 1 (January 19): 31.
Cary, M.P., Jr., V. Goode, N. Credo, et al. 2018. Hospital readmissions among total hip replacement patients in 2009 and 2014. Archives of Physical Medicine and Rehabilitation (January 30).
Dharmarajan, K. Y. Wang, Z. Lin, et al. 2017. Association of changing hospital readmission rates with mortality rates after hospital discharge. Journal of the American Medical Association 318, no. 3 (July 18): 270-278.
Gupta, A., L.A. Allen, D.L. Bhatt, et al. 2017. Association of the Hospital Readmissions Reduction Program implementation with readmission and mortality outcomes in heart failure. JAMA Cardiology (November 12). https://jamanetwork.com/journals/jamacardiology/article-abstract/2663213?redirect=true.
Himmelstein, D., and S. Woolhandler. 2015. Quality improvement: ‘Become good at cheating and you never need to become good at anything else’. Health Affairs blog, August 27. http://healthaffairs.org/blog/2015/08/27/quality-improvement-become-good-at-cheating-and-you-never-need-to-become-good-at-anything-else/.
Ibrahim, A.M., J.B. Dimick, S.S. Sinha, et al. 2017. Association of coded severity with readmission reduction after the Hospital Readmissions Reduction Program. JAMA Internal Medicine (November 13). https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2663252.
Klevens, R.M., J.R. Edwards, C.L. Richards, Jr., et al. 2007. Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Reports 122, no. 2 (March-April): 160-166.
Medicare Payment Advisory Commission. 2018. Medicare and the health care delivery system. Washington, DC: MedPAC.
Medicare Payment Advisory Commission. 2016. Report to the Congress: Medicare payment policy. Washington, DC: MedPAC.
Medicare Payment Advisory Commission. 2013. Report to the Congress: Medicare and the health care delivery system. Washington, DC: MedPAC.
Medicare Payment Advisory Commission. 2008. Report to the Congress: Reforming the delivery system. Washington, DC: MedPAC.
Rockwood, K. 2012. Hospitalization and effects on cognition. Neurology 78, no 13 (March 27): e86-87.
Wilson, R.S., L.E. Hebert, P.A. Scherr, et al. 2012. Cognitive decline after hospitalization in a community population of older persons. Neurology 78, no. 13 (March 27): 950-956.
Zuckerman, R.B., S.H. Sheingold, E.J. Orav, et al. 2016. Readmissions, observation, and the Hospital Readmissions Reduction Program. New England Journal of Medicine 374, no. 16 (April 21): 1543-1551.
