Today, the Commission published its comment letter to the Centers for Medicare and Medicaid Services (CMS) on the fiscal year 2016 hospice proposed rule. In the rule, CMS proposed modifying the structure of payment rates for hospice routine home care. The proposed changes, though modest, are consistent with the Commission’s March 2009 recommendation for hospice payment reform. The Commission urges CMS to proceed with implementing these changes.
Medicare’s hospice benefit was established in 1983 in part to provide Medicare beneficiaries with an alternative approach to care at the end of life consistent with the preferences of those who do not want intensive medical interventions. Hospice permits beneficiaries at the end of life to opt for a death at home, surrounded by friends and family, rather than in an institutional clinical setting.
The Commission recognizes the importance of hospice and its substantial contribution to end-of life care for beneficiaries. However, it is concerned that the current payment system may be incentivizing inappropriate use of the hospice benefit. The hospice payment system currently pays hospice providers a flat per diem rate. The Commission has pointed out that this payment structure does not reflect the actual cost of providing hospice care: costs are higher at the beginning and end of a hospice episode, and lower during the middle of an episode. This U-shaped cost curve reflects hospices’ higher service intensity at the time of the patient’s admission and the time surrounding the patient’s death. However, a flat per diem payment does not differentiate between the beginning, middle, and end of an episode. As a result, relative to costs, the daily payment rate is too low at the beginning and end of an episode and too high in the middle of an episode. This structure means that long hospice stays are particularly profitable for providers, because the “middle” of these stays, when costs are relatively low, are longer. In contrast, short stays may be unprofitable, because providers have little opportunity to recoup their beginning- and end-of-episode costs, given the short intervening period of relatively lower costs.
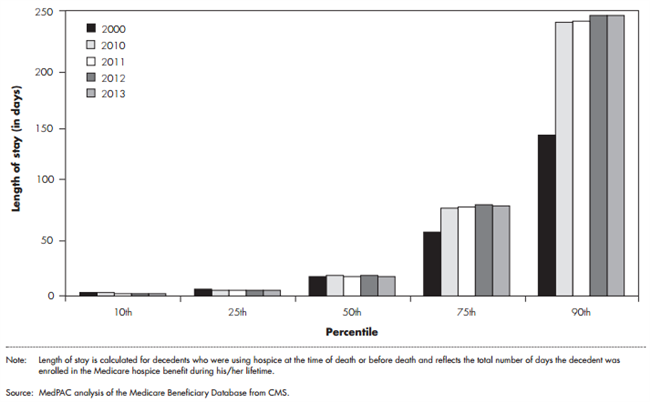
This payment structure may be spurring some providers to pursue business models that maximize profit by enrolling patients more likely to have long stays. In part reflecting these incentives, average length of stay grew from about 54 days to 88 days between 2000 and 2012. The increase in average length of stay observed since 2000 is largely due to an increase in very long hospice stays, while short stays remained virtually unchanged (figure 1). Some argue that length of stay has increased because of a shift in diagnoses among hospice enrollees towards conditions that tend to have long lengths of stay. However, our analysis shows that lengths of stay were longer in for-profit providers than not-for-profit providers across all diagnoses, suggesting that increases in lengths of stay may be driven in part by financial incentives rather than purely clinical factors.
Figure 1. Long hospice stays got longer between 2000 and 2013
 In March 2009, the Commission recommended that the hospice payment system be changed from a flat per diem payment to one in which the payment is higher at the beginning and end of the episode (in the last days of life) and lower in the middle. PPACA gave CMS the authority to make budget-neutral revisions to the hospice payment as the Secretary of Health and Human Services determines appropriate, beginning in fiscal year (FY) 2014 or later.
In March 2009, the Commission recommended that the hospice payment system be changed from a flat per diem payment to one in which the payment is higher at the beginning and end of the episode (in the last days of life) and lower in the middle. PPACA gave CMS the authority to make budget-neutral revisions to the hospice payment as the Secretary of Health and Human Services determines appropriate, beginning in fiscal year (FY) 2014 or later.
In the FY2016 hospice proposed rule, CMS has proposed a new structure for routine home care (RHC) payments (Hospice days are sorted into four categories, each with its own per diem rate – the RHC category is by far the most common category, representing more than 98 percent of hospice days). CMS has proposed a higher base rate for RHC during the first 60 days of an episode ($188) and a lower base rate for days 61 and beyond ($147). In addition to the per diem payments, CMS has proposed to make additional payments, referred to as service intensity adjustment (SIA), for certain skilled hospice visits that occur during the last seven days of life.
The payment structure that CMS has proposed would begin to better align payments with the u-shaped pattern of hospice visits throughout an episode. Although the payment changes included in this proposal would generally have a modest impact on providers (as reflected in CMS’s impact analysis), these changes would begin to address some of the negative consequences that have resulted from the misalignment between payment and costs under the current flat per diem payment system. The Commission therefore urges CMS to move quickly to finalize and implement changes to the RHC rates for FY2016.
For more detailed comments, check out the Commission’s full comment to CMS.
